Cordlife Philippines Earns Back-to-Back AABB reaccreditation and ISO recertification

Cordlife Philippines Earns Back-to-Back AABB reaccreditation and ISO recertification
We’re proud to share that Cordlife Philippines has once again achieved AABB reaccreditation and ISO 9001:2015 recertification, a testament to our unwavering commitment to world-class stem cell banking services.

The AABB (Association for the Advancement of Blood and Biotherapies) accreditation recognizes excellence in cellular therapy services. This international gold standard confirms that our quality and operational systems meet and even exceed the rigorous requirements set by the AABB Standards Committees.

Meanwhile, the ISO 9001:2015 certification from SGS highlights our consistent ability to deliver products and services that meet both customer expectations and strict regulatory requirements, backed by a strong quality management system.

With these recognitions, Cordlife Philippines remains the first and only cord blood bank in the country to hold both prestigious credentials, a distinction we’ve proudly maintained since 2017 for AABB and 2012 for ISO.
For every family we serve, these seals are more than just certificates. They are our promise to provide the highest standards of service, processing, and long-term storage for your child’s umbilical cord blood stem cells – today and for years to come.
Learn more about stem cell banking today
Unlock essential knowledge about umbilical cord stem cell banking and be more prepared for the arrival of your little one with Cordlife Philippines' Information Pack.
Recent Blog Posts
- 20 August 2025
- 04 August 2025
- 07 July 2025
- 16 June 2025
- 16 June 2025
Katrina Grace Castro's 10-Year Journey at Cordlife Philippines

Spotlight on Excellence: Katrina Grace Castro's 10-Year Journey at Cordlife Philippines
As Cordlife Philippines commemorates its 15th anniversary, we are privileged to highlight the remarkable journey of one of our esteemed team members, Katrina Grace Castro. With a decade of unwavering dedication and expertise, Katrina has played a pivotal role in Cordlife Philippines’ commitment to revolutionize healthcare and empower families across the country. Join us as we delve into Katrina's inspiring story and gain insights into her invaluable contributions to Cordlife Philippines.

Q&A Spotlight
1. Can you share briefly your 10-year journey at Cordlife Philippines? What is your day-to-day like?
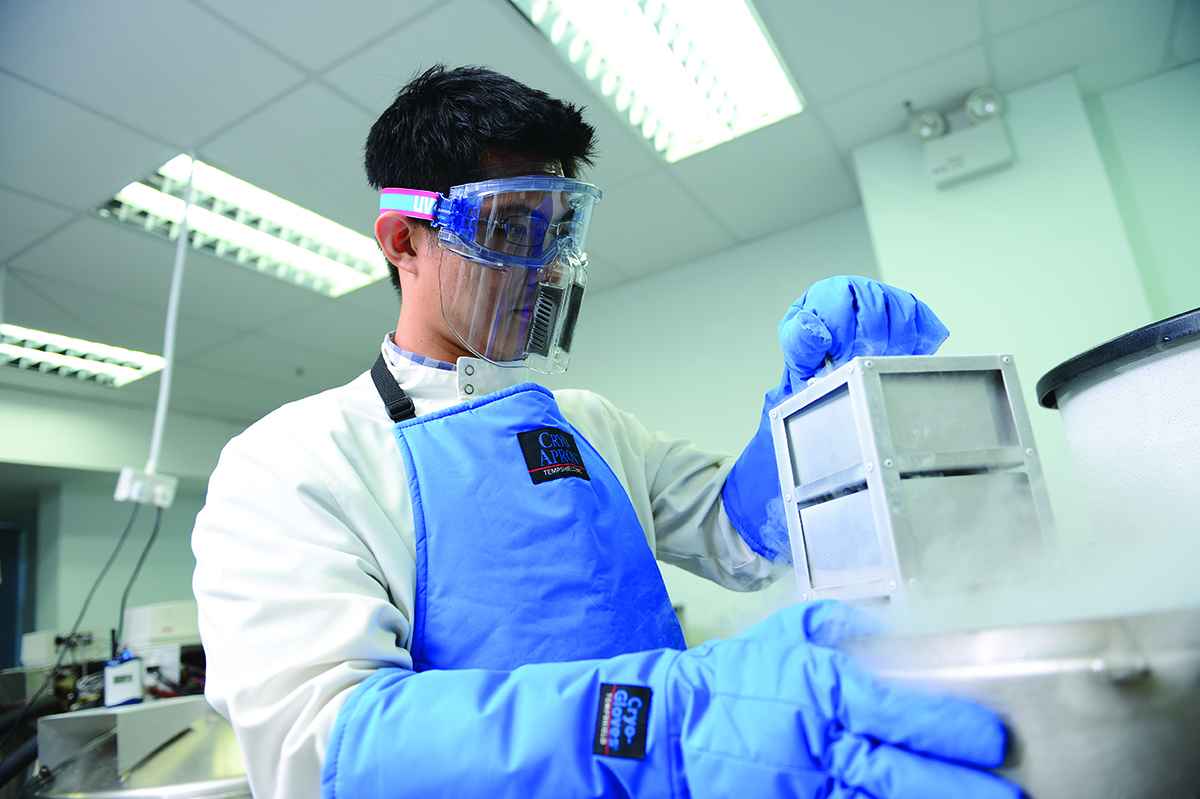
Katrina: My job is to oversee the operations in the Cordlife Philippines laboratory and to ensure our compliance to local and international standards. I also assist our senior manager in budget planning.
I joined Cordlife Philippines in 2013, starting my journey as a laboratory biotechnologist. My team is responsible for processing cord blood and tissue samples. We ensure that our laboratory and all equipment, especially our cryostorage tanks, are always in the best condition.
2. As the assistant manager of the Laboratory department, what are common misconceptions about your job?
Katrina: That our work is repetitive and somewhat routinary. But in reality, we work on various projects beyond processing of stem cells that are intellectually stimulating.
Among these projects are the enhancement of our cryostorage capabilities, the ongoing augmentation of Cordlife Philippines’ clinical laboratory, and our steady preparation and planning for our regular audits.

3. What do you love most about what you do for Cordlife Philippines?
Katrina: I believe in our mission of providing reliable healthcare solutions through innovation, technological advancement, and commitment to quality and in the value of what we do. We help our clients in securing the health of their families through our umbilical cord stem cell banking and healthcare services.
4. What valuable insights or lessons would you like to pass on to your younger peers from the Lab Team?
Katrina: To always have a positive attitude. No matter how hard our job is, if you have the right attitude and mindset, the work will become easier. And to always think of the importance of what we do. Our clients entrust us with their precious cord blood, cord tissue, and cord lining stem cell samples, we must handle them carefully and treat them as if they are our own.
5. As Cordlife Philippines continues to expand its horizons, what exciting developments or opportunities are you eagerly anticipating in the future?
Katrina: We are incredibly excited about the upcoming developments in our laboratory department at Cordlife Philippines! I mentioned earlier that one of our main projects on the horizon is expanding our cryostorage capabilities. This involves not only purchasing new cryotanks but also meticulously validating them to ensure they meet the highest standards of quality and reliability.
Additionally, we're implementing a proactive approach to the preventive maintenance of our cryotanks, ensuring optimal performance.
But that's not all – we're also exploring other sources of stem cells to broaden our potential avenues for healthcare innovation. With our sights set on the future, we're eager to implement more cutting-edge technology and research to enhance our services and impact even more lives positively.
Furthermore, the ongoing development and improvement of our clinical laboratory, which has been launched this 2024, marks a significant milestone in our journey. This expansion strengthens our ability to provide comprehensive diagnostic services, offering our clients even greater convenience and peace of mind.
Amidst all these, we remain committed to maintaining the highest of standards in our offerings. We continuously gear up for the regular ISO:9001 certification and AABB accreditation, further solidifying our reputation for adherence to the highest standards of quality and safety.
These projects in the pipeline represent our unwavering dedication to pushing the boundaries of healthcare innovation and ensuring the well-being of Filipino families for years to come.

Katrina Grace Castro exemplifies the dedication, expertise, and passion that define Cordlife Philippines' commitment to excellence. As we celebrate 15 years of innovation and impact, we extend our deepest gratitude to Katrina and all our team members for their unwavering dedication.
Together, we continue to shape the future of healthcare and empower families nationwide.
Recent Blog Posts
- 20 August 2025
- 04 August 2025
- 07 July 2025
- 16 June 2025
- 16 June 2025
Celebrating 15 Years of Healthcare Innovation with Cordlife Philippines

Celebrating 15 Years of Healthcare Innovation with Cordlife Philippines
As we mark our 15th anniversary, we at Cordlife Philippines are honored to look back on our journey of trailblazing innovations in the healthcare industry. Since our inception, we have been at the forefront of introducing groundbreaking advancements, shaping the landscape of healthcare in the Philippines.

Pioneering Innovation
Fifteen years ago, we proudly launched the country's first private umbilical cord stem cell bank, laying the foundation for a new era of healthcare possibilities.
Over the years, we have introduced numerous firsts to empower Filipino families with cutting-edge healthcare solutions both in the umbilical cord stem cell banking sphere and genetic screening space. Our ever-evolving and ever-improving umbilical cord stem cell banking and genetic screening services such as cord blood banking, cord lining banking, cord tissue banking, mesenchymal stem cell banking, non-invasive prenatal testing (NIPT), baby genetic screening, and chromosomal microarray analysis (CMA) test, have been shaped with the needs of our clients in mind.
Commitment to Quality
Our commitment to excellence is unwavering, as evidenced by the consistent stamp of approval from ISO:9001 certification, AABB accreditation, and DOH license approvals. These certifications reflect our dedication to upholding the highest standards of service and care for our clients.
Gratitude for Your Support
We extend our heartfelt gratitude to our valued partners and clients for their unwavering support throughout our journey. Your shared vision for the betterment of Filipino families' lives has been instrumental in our success.
Expanding Horizons - the Next 15
We remain steadfast in our resolve to overcome obstacles and continue making a positive impact in all the lives we touch. As we embark on the next chapter of our journey, we are excited to expand our portfolio in bio-banking, stem cell expansion, diagnostics, and genetic testing. Additionally, we plan to introduce offerings in women's wellness and family lifestyle solutions, further enriching the lives of Filipino families.
Join Us in Shaping the Future
We invite you to join hands with us once again as we enter the next 15 years of our exciting journey. Together, let's reshape and revolutionize the Philippine healthcare industry, ensuring a healthier and brighter future for generations to come.
Thank you for your continued trust and support. Here's to celebrating 15 years and beyond of helping people live healthier, happier, and longer lives!
Recent Blog Posts
- 20 August 2025
- 04 August 2025
- 07 July 2025
- 16 June 2025
- 16 June 2025
The Power of Cord Blood Banking: What Every Expecting Mother Needs to Know

The Power of Cord Blood Banking: What Every Expecting Mother Needs to Know
Bringing a new life into the world is a remarkable journey filled with joy, anticipation, and a plethora of decisions to make. One decision that is gaining prominence among pregnant mothers is the option of cord blood banking. Get to know why it's something every expecting mother should consider.
What is cord blood and what are cord blood stem cells?
Cord blood is the blood that remains in the umbilical cord after a baby is born. It is a rich source of hematopoietic stem cells or HSCs, which have the ability to differentiate into different types of cells in the body such as red blood cells, white blood cells, and platelets. These cells are the building blocks of life and are crucial for the development and repair of tissues and organs.
HSCs have unique properties that make them useful for medical treatments. They can be used to treat critical illnesses, including certain cancers like leukemia, blood disorders such as thalassemia and anemia, and metabolic disorders. The ability of these cells to regenerate and differentiate makes them a powerful tool in stem cell therapy.
What is the process of cord blood banking with Cordlife Ph?
Cordlife Philippines offers cord blood banking – the process of collecting, processing, and storing of stem cells from a baby’s umbilical cord upon birth.
It is safe and painless both for the mother or the baby. Once collected, the cord blood is processed and cryopreserved at Cordlife Philippine’s local facility in UP AyalaLand Technohub in order to maintain its potency for potential future use and protection of the whole family.
Cord blood banking as a health protection for the whole family
One of the most significant advantages of cord blood banking is that the banked stem cells are a perfect match for the baby or the owner of the stem cells and may also be a match for siblings and parents. This means that in case of a medical need, the family has a readily available source of compatible stem cells, getting rid of the challenges that come with finding a suitable match from public banks.
While no one wants to think about potential health issues, having access to banked stem cells can provide peace of mind, knowing that you've taken a proactive step towards ensuring your child's well-being even before they are born.
What other benefits come with cord blood banking with Cordlife Philippines?
Apart from the storage of stem cells, Cordlife PH offers a wide range of complimentary value-added services, including its pregnancy insurance, Cordlife Shield. This insurance covers the mother as early as 18 weeks of pregnancy against some of the most common pregnancy complications, like eclampsia and pre-eclampsia, and the baby from congenital illnesses from birth until the 6th month of age.
Cord blood banking with Cordlife Philippines also entitles you to a free membership in Cordlife ALLIANCE, the first-ever community cord blood banking program in the Philippines.
If a family's cord blood isn't suitable in case of a medical need, the family can access a diverse pool of banked cord blood units from other Asian countries where Cordlife operates to search for an alternative match.
Other free benefits of cord blood banking with Cordlife PH include Cordlife Baby Genetic Screening, Transplant Care, Cordblood Network, and more.
As you embark on this incredible journey of motherhood, consider the power of cord blood banking as a gift to your child's and family’s future. The decision to bank cord blood is a proactive step that may offer life-saving benefits and peace of mind. Ask your OB-GYN about cord blood banking today or learn more by claiming a free and non-obligatory consultation with our consultants.
Recent Blog Posts
- 20 August 2025
- 04 August 2025
- 07 July 2025
- 16 June 2025
- 16 June 2025
Endometriosis
Endometriosis
By Dr. Christopher Ng
Obstetrician and Gynaecologist
GynaeMD Women’s & Rejuvenation Clinic, Camden Medical Centre
MBBS (London, UK), FRANZCOG (Aust-NZ), MMed (S'pore), FAMS (S'pore)
What is endometriosis?

What is endometriosis?
Endometriosis is a common medical condition characterised by growth of endometrium (the tissue that normally lines the uterus) beyond or outside the uterus. It looks and acts like tissue in the uterus. It most often appears in places within the pelvis:
- Ovaries
- Fallopian tubes
- Surface of the uterus
- Cul-de-sac (space behind the uterus)
- Bowel
- Bladder and ureters
- Rectum
Endometrial tissue can attach to organs in the pelvis or the peritoneum, which lines the inside of the pelvis and abdomen. In rare cases, it can also be found in other parts of the body. Endometrial tissue that grows in the ovaries can result in the formation of an endometriotic cyst.
Endometrial tissue outside the uterus responds to hormonal changes. During the menstrual cycle, it breaks down and bleeds similarly to the uterine lining. The breakdown and bleeding of this tissue each month can result in scar tissue known as adhesions.
Adhesions can cause pain and sometimes bind organs together.
The symptoms of endometriosis often worsen over time. In many cases, treatment can prevent the condition from worsening.
What causes endometriosis?
The causes of endometriosis are still unknown. People often think that this is because the blood from the period flows backwards into the pelvic cavity.

What are the signs and symptoms of endometriosis?
Women may complain of the following:
- Heavy and sometimes irregular menses
- Painful periods
- Pain during sex (this is a deep pain during penetration)
- Pain in the pelvis or lower abdomen in between periods
- It may be associated with infertility.
30–40% of women with endometriosis will have trouble getting pregnant after a year of regular sexual activity. Age-dependent cycle fecundity (monthly) rates in healthy fertile women range between 15% and 25%. That chance is less than 1% for women with severe endometriotic disease.
How common is endometriosis?
Endometriosis affects 5% to 20% of women of reproductive age and is the cause of infertility in 30 to 40% of women with endometriosis.

Is there a specific age group that is more susceptible to endometriosis?
It is more common in women between the ages of 20 and 40. According to the literature, Caucasian women are more likely than Afro-Caribbean women to develop endometriosis.
Is there a cure for endometriosis?
Endometriosis is hormonally related, so there is no permanent cure short of natural menopause or surgical menopause (by removing the ovaries); but even then, there are reports of endometriosis in menopausal women, though this is rare. There are, however, treatments available to help women manage and deal with their symptoms. In some women, pregnancy can alleviate the symptoms and effects of endometriosis. Endometriosis symptoms are usually lessened by pregnancy and hormonal drug treatments, but neither of these cures the disease.
Symptoms may or may not recur after childbirth. Breastfeeding can help most women postpone the return of symptoms, but only if it is frequent and intense enough to suppress the menstrual cycle. Doctors sometimes advise women with endometriosis not to delay having children because the condition tends to worsen over time. The longer you have endometriosis, the more likely you are to become infertile.

How is endometriosis diagnosed?
In addition to a thorough history, a pelvic exam will be done to see if you have any of the typical signs of endometriosis. This is done to try to pinpoint the source of the pelvic pain. Other potential causes of pelvic pain must be ruled out. Endometriotic cysts can be detected using a pelvic ultrasound scan, which is usually combined with a blood CA125 test (which can be high in women with endometriosis).
Endometriosis can be mild, moderate, or severe. A laparoscopy, also known as a keyhole surgery, can be used to look directly inside the pelvis to determine the extent of the disease. This procedure will be carried out while under general anesthesia. Endometriotic lesions, endometriotic cysts, and adhesions can all be removed during a laparoscopy.
What are the surgical and non-surgical treatment available?
Treatment focuses on either pain relief or infertility. Some pain relief options are as follows:
- Analgesics (Pain killer)
- Combined oral contraceptive pill
- Progression intrauterine device (Mirena)
- Danazol (Amle hormone compound)
- Oral progesterone (Visanne)
- Depot progesterone injections (Depoprovera)
- Gonadotropin-releasing hormone (GnRH) agonists — to create a tesendo menopausal state
They are all equally effective, but their side effects and cost profiles are different. Endometriosis-related pain is reduced when ovarian function is suppressed for several months with any of these medications.
Surgery may be recommended for some women whose medical treatment has not relieved their pain or infertility. Surgery is done to remove or coagulate all endometriotic peritoneal lesions, endometriotic ovarian cysts, deep rectovaginal endometriosis, and related adhesions, and to restore normal anatomy. Ablation of endometriotic lesions combined with removal of endometriotic adhesions improves fertility in endometriosis. Laparoscopic surgery nearly doubles the chances of pregnancy and live birth for women with mild endometriosis when compared to not having the surgery. Following surgery, pregnancy rates for women with mild endometriosis as their only fertility problem range between 81% and 84%. Those with moderate to severe endometriosis, including damage to the ovaries, have a 36% to 66% chance of getting pregnant after surgery. Endometriosis often comes back after treatment, so pregnancy rates are highest in the year after surgery.
Also, women who can't get pregnant after surgery may need SOIUI (superovulation intrauterine insemination) or IVF (in vitro fertilisation). SOIUI improves fertility in women with minimal to mild endometriosis, but tubal patency is required. IVF is a good treatment option, especially if the tubes are blocked, if male factor infertility is present, or if other treatments haven't worked.
Recent Blog Posts
- 20 August 2025
- 04 August 2025
- 07 July 2025
- 16 June 2025
- 16 June 2025
Do pregnant women need fish oil supplementation?
Do pregnant women need fish oil supplementation?
By Dr. James Lee
MBBS, MRCOG, FAMS, GDip

It is important that a pregnant woman should not consume any medication, herbal product or health care supplement unnecessarily or in excess, unless there is strong evidence that she needs it to improve the health of the pregnancy and/or the fetus inside her womb. The use of fish oil during pregnancy and breastfeeding remains contentious. Pregnant women are advised to understand the potential benefits and ills when they decide to take fish oil supplement.
What is fish oil?
Fishes that flourish in cold “temperate” oceans have generally higher content of oil in their muscles and organs. Fish oil comprises mainly omega-3 fatty acids, and DHA and EPA are the two most important omega-3 fatty acids. Omega-3 fatty acids are important building blocks of fatty tissues in human, such as the gray matter of the brain, the light receiving layer (retina) of the eyes and the extensive nerve network.
Why are Omega-3 fatty acids important during pregnancy & breastfeeding?
The critical window when DHA is taken up into these tissues is between the second half of pregnancy and the first two years of life. When animals were fed with diet deficient in DHA, the studies found that the vital nerve organs formed had a different fatty acid composition (with higher omega-6 fatty acids). These changes in fatty acid composition gave lasting negative effects on learning behaviour, brain metabolism, nerve formation and visual functions. These neural changes could not be reversed even when subsequent omega-3 fatty acid treatment successfully return the composition to what it should be. We cannot ignore the significance of adequate omega-3 fatty acid accretion into neural tissue during this window period. Optimizing neural tissue development is by far the most important function of omega-3 FAs in the perinatal period. Nevertheless, omega-3 FA deficiency in pregnancy has been associated with preterm labor, increased risk of postnatal depression, increased tendency of the offspring to develop asthma and other allergic conditions.
What are the natural sources of Omega-3 FA?

The basic omega-3 FA is ALA (alpha-linolenic acid), from which the functionally important omega-3 fatty acids like DHA and EPA are derived. In nature, DHA and EPA are mostly found in fatty fish such as salmon, tuna, sardines and trout. ALA, on the other hand, is a major component of some plant oil,such as canola oil and flaxseed oil. The idea of consuming ALA in large amount of plant oil, so that the body can make DHA and EPA to incorporate them into the brain, is possible, but highly inefficient. The conversion process demands a lot of chemical energy in the body and is extremely slow. Consuming pre-formed DHA and EPA is the better option.
Pregnant women are advised not to eat too much fish!
Years of industrialization have polluted the oceans, by pumping industrial chemicals and toxic wastes directly into the ocean, or by first polluting the atmosphere before poisoning the seas via the rain. Significant levels of mercury, polychlorinated biphenyls (PCBs) and dioxin have been found concentrated in oily ocean fishes. The bigger fishes that survived years of ocean living are more contaminated. These pollutants are toxic to the nerve tissues, especially while the nerves are maturing, and the growing fetus is therefore extremely vulnerable. The pregnant women are to stay away from eating large oily fish, such as shark, swordfish, marlin and king mackerel. In fact, UK and US authorities have advocated restricting their pregnant women to two fish meals a week (i.e. about 340gm a week). Fishes that are bred in the tropics are usually are less contaminated.
On the other hand, the adequate consumption of omega-3 fatty acid is essential for fetal brain growth. On weighing all sides, most authorities proselytise that the health benefits of pregnant women eating fish with low level of mercury contamination outweigh the risks of the pollutants.
Pregnant women are encouraged to eat fish with low mercury contamination, to remove the skin and fat prior to cooking. They are advised against eating raw fish or shellfish, instead, baking, broiling, steaming the fish will reduce the industrial pollutant level.
If not from fish, where else can I get enough Omega-3s?
Pregnant women who do not eat fish, who are not keen to take them while pregnant, or are eating mainly non-oily fish (tropical species), may obtain their omega-3 fatty acids by fish oil pill. The fish oil supplements should be packaged with purified fish oil, so that the PCBs and dioxin contaminants are removed. There are many formulations of fish oil supplements, their characteristics may affect their efficacy, although to date, the claims are not sufficiently researched. The consensus however is to take between 200mg and 300mg of omega-3 fatty acids a day.
What about fish liver oil?
Pregnant women ought not to consume fish liver oil, such as cod liver oil. Fish liver is the main organ where mercury is detoxified and therefore has the highest concentration of the pollutant. Besides, vitamin A (which is fat soluble) is largely stored in the liver, and thus the liver has the highest level of vitamin A in the body. Excessive vitamin A usage in pregnancy is associated with fetal malformation.
Does fish oil supplementation make better babies?
The potential effects of DHA supplementation in pregnancy on early childhood development are promising. Evidence from animal studies and observational surveys has found improved visual response, brain functioning and childhood intelligence scores. Increased DHA in baby’s blood at birth has also been correlated with reduced incidence of childhood allergic diseases such as asthma, atopic dermatitis and allergic rhinitis.
Several interventional randomized controlled trials have been organized to verify these benefits. Some of them have been going on for several years, and their interim results published. To date, the conclusions have been inconsistent; some studies showed beneficial outcomes with DHA supplementation, whereas others found no advantage. This is not unexpected as the study design and the result analysis have to consider many confounding factors that affect the baby’s development and functioning.
Unfortunately we have as yet no consistent proof that fish oil supplementation will give clinical benefits to the children as they grow older. What has been established is the safety of using fish oil supplementation in pregnancy and during breastfeeding. We look forward to more evidence of its clinical effectiveness in the coming years.
Recent Blog Posts
- 20 August 2025
- 04 August 2025
- 07 July 2025
- 16 June 2025
- 16 June 2025
Gynaecology and the beauty of life
Gynaecology and the beauty of life
By Dr. Alex Ooi
MBBS, MMed (O&G), FRCOG, FAMS, FICS, MBA

Stem cell technology and applications are advancing rapidly, and their storage is insurance in the sense that you hope to never need their potential life-giving benefits. However, the practical reality of progenitor cells' ability to correct a disease is a stark reminder of how fragile human creation is and how much we take our bodies for granted when they are in good health.
When I was asked to write an article, I thought about my work experiences and decided to do something simple and not academic for a change. I chose to write about appreciating the beauty that comes from nature and life.
My pursuit of a career resulted in that career becoming a part of my life, and I'm still loving every minute of it more than 30 years later. Managing patients' problems, as well as interactions with them and their relatives who accompany them on visits, have both served as an inspiration and a source of a lifestyle philosophy.

Sleepless nights while delivering a baby, performing caesareans or major pelvic surgeries can be stressful, but what in life isn't? Stress is necessary for life and gives it meaning. Patients who embrace and use it to achieve positive outcomes handle their problems much better. Those who seek a “stress-free life” are trying to achieve an unattainable goal, which often delays illness recovery. Some people find simple tasks to be very stressful, while others find them to be very easy. Positivity prevails when the latter attitude is adopted.
In the course of healing illnesses and managing difficult transitions, I sense that many patients also want to look and feel good. As a result, I began incorporating simple life-improvement protocols for both physical and mental wellbeing. My interest in keyhole surgery led me to expand my services to include liposuction or fat transfer — a natural extension of the main surgical discipline that involves working through small openings for a major outcome.
The oft-heard adage “age is just a number” is a good one to live by. Patients who take action to manage their hot flushes, tissue laxity, loss of libido, wrinkles, pigmentation, aches and pains, hair loss, fat in unwanted places, and other non-health issues are much better off. Patients who complain about reaching 50, 60, or even 40 and do nothing to resolve the issues appear to be stuck in dissatisfaction. Those who have realistic expectations and are aware that any medical and lifestyle advances made are only to postpone the inevitable effects of ageing (which is a gain in and of itself), are happier in life.
This one life we have, while full of dangers and problems, is also full of joy and rewards. There's no need to push the boundaries of indulgence in order to keep up with the Joneses. The needs for living a full life are simple, easily attained, and readily enjoyed by maintaining a positive attitude and being grateful for the many mercies we receive from moment to moment. Talking about “needs” leads me to the other two ingredients of youthfulness.

Regular exercise
Patients who know that a car needs its cylinders greased, tyres inflated, and tank filled can live a fuller life with less illness by engaging in regular, effective exercise. This is vital as we age. My workout consists of cross-training, stretching, and crunches in the gym. Choose one that works for you and make time for exercise every day. Not only is it good for your health, but it will also make you feel (by releasing endorphins) and look good. Even my younger patients who don't work out have a harder time giving birth or going through major surgery. Furthermore, these patients are frequently overweight, which presents its own set of challenges. The body isn't able to handle these stresses as well as it used to, and this is even worse for older patients. As we age, we become less active and use less energy, so we need to exercise more.

Eating well
When it comes to eating well, it's not about how rich or expensive the food is, but about choosing natural foods with fewer calories and fat. This doesn't imply a lack of variety, as there is a wide range of good food available. It can be hard to start and keep up, but once you do, you'll get to be healthier and look younger. Many patients who do well also consider taking supplements and avoiding medications and vitamins. And, of course, quit smoking and limit your alcohol intake. Maintain a positive attitude, exercise regularly, and eat healthily. These, along with managing one's disposition and self-image, will go a long way toward preventing illness and hastening recovery.
Recent Blog Posts
- 20 August 2025
- 04 August 2025
- 07 July 2025
- 16 June 2025
- 16 June 2025
Vaginal infections
Vaginal infections
By Dr. Wong Heng Fok
Consultant Obstetrician & Gynaecologist, Urogynaecologist
MBBS (Singapore), MRCOG (London, UK)

Many women suffer in silence, unknowingly. In this article, Dr Wong H.F. shares with us his knowledge of Vulvovaginitis, also known as vaginal infection in women.
1. Thrush/Fungus
When doctors say "yeast," we usually refer to the fungus Candida albicans. It's commonly found on the skin and in the gastrointestinal tract anywhere from the mouth to the anus.
Candida can live in the vagina of up to one in five healthy women of childbearing age without causing any symptoms. Most of the time, a healthy vaginal environment and a normal immune system prevent the harmless yeast from overgrowing and causing vaginitis. A yeast infection occurs when there's an abundance of yeast. It completely overwhelms the vaginal defence system.
Yeast infections can cause a wide range of symptoms. In general, the more intense the itching and redness, the greater the presence of yeast organisms. In some women, secretions predominate, with profuse discharge that adheres to the vaginal wall in thick white patches or white plaques. This is also referred to as vaginal thrush. Odour is not a common complaint, though candida can cause a yeasty odour in some women.
This condition is usually diagnosed with a simple pelvic examination in which the vaginal discharge is swabbed and sent for culture.
Treatment usually consists of a combination of vaginal pessaries available on the market for one to seven days. We usually apply an anti-fungal/steroid cream to relieve local itchiness. If you have recurrent or persistent fungal infections, they can be difficult to treat, and you should see your GP or gynaecologist to confirm the diagnosis and rule out other conditions, such as bacterial vaginosis, which is just as common as fungal infections.
2. Bacterial vaginosis (BV)
This condition is as common as yeast/thrush or fungal infection and manifests as vaginal discharge (which may be yellow green as opposed to white discharge in yeast infection). The difference between fungal infections and BV is that BV discharge is foul-smelling with a fishy odour and is the leading cause of unpleasant odours. It may also cause pain and irritation around the vulva.
We can usually confirm the diagnosis by obtaining a vaginal swab and sending it to the laboratory. In the meantime, we usually order vaginal pessaries or even oral medication for 7 to 10 days. The most common are Gardnerella and Trichomonas infections.
BV, like yeast infections, is not a sexually transmitted infection, but rather a bacterial imbalance in the vaginal environment. You should see a gynaecologist or a GP for treatment.
3. Sexually transmitted disease (STD)
There are numerous STDs to discuss, but we will only cover the most common ones here.
i) Herpes infection
Herpes simplex virus (HSV) infections are very common all over the world. HSV-1 is the most common cause of herpes infections on the lips and mouth, including cold sores and fever blisters. It is spread by kissing. HSV-1 can also cause genital herpes, but HSV-2 is the most common cause. HSV-2 is contracted through sexual contact. You could be infected with HSV-1 or HSV-2 but have no symptoms. Symptoms are often brought on by exposure to the sun, fever, menstruation, emotional stress, illness, or a weak immune system.
Herpes has no cure and is likely to reoccur. However, some people may have one outbreak and never have another.
Genital herpes causes multiple painful blisters and ulcers around the vulva and perineum (area immediately next to the vagina) and, in severe cases, may cause difficulty passing urine due to pain
Most of the time, your doctor will be able to tell if you have herpes just by looking at you. However, if your doctor is unsure, he or she may take a sample from the blisters to test for the virus.
Antiviral drugs might help shorten the length of a herpes outbreak and stop it from happening again. We give oral tablets and a topical antiviral cream for a week. Some patients require admission due to the severity of their ulcers.
ii) Chlamydiae
Chlamydiae is a common sexually transmitted disease (STD) caused by the bacterium Chlamydia trachomatis that can damage a woman's reproductive organs. Even if the symptoms of chlamydia are usually mild or absent, serious complications that cause irreversible damage, such as infertility, can occur "silently" before a woman is aware of a problem. Chlamydia can also cause discharge from the penis of an infected man.
Chlamydia is the most commonly reported bacterial sexually transmitted disease in the United States, particularly among young girls.
Anyone who engages in sexual activity can become infected with chlamydia. The greater the number of sex partners, the greater the risk of infection. Teenage girls and young women are especially vulnerable to infection if sexually active because their cervix (opening to the uterus) is not fully mature and is likely more susceptible to infection.
Chlamydia is known as a "silent" disease because the majority of infected people show no symptoms. If symptoms do appear, they usually do so 1 to 3 weeks after exposure.
In women, the bacteria first infect the cervix and urethra (urine canal). Women experiencing symptoms may experience abnormal vaginal discharge or a burning sensation when urinating. If the infection spreads from the cervix to the fallopian tubes (tubes that carry fertilised eggs from the ovaries to the uterus), some women have no symptoms, while others have lower abdominal pain and fever.
If a woman doesn't get treatment for an infection, it can spread to the uterus or fallopian tubes and cause pelvic inflammatory disease. This occurs in about 10 to 15 percent of women with untreated chlamydiae and may lead to fertility issues later in life.
Chlamydia can be easily treated and cured with antibiotics. A single dose of azithromycin or a week of doxycycline (twice daily) are the most commonly used treatments.
When an STD is discovered, contact tracing of the male partner is needed, and all sex partners must be evaluated, tested, and treated.
iii) Gonorrhoea
Gonorrhoea is a sexually transmitted disease (STD) caused by Neisseria gonorrhoeae, a bacterium that thrives in the warm, moist environment of the reproductive tract.
Anyone who engages in sexual activity is at risk of contracting gonorrhea.
The symptoms of gonorrhea in women are frequently mild, and the majority of infected women have no symptoms at all. Even when a woman experiences symptoms, they can be so non-specific and can be mistaken as a bladder or vaginal infection. Some of the first symptoms and signs in women are pain or burning when they urinate, more discharge from the vaginal canal, or bleeding between periods.
Gonorrhoea can lead to pelvic inflammatory disease (PID), which can cause internal abscesses (pus-filled “pockets” that are hard to treat) and long-term, chronic pelvic pain. PID can damage the fallopian tubes enough to cause infertility or increase the risk of ectopic pregnancy.
Again, a vaginal swab can easily diagnose the condition, and antibiotics can treat it. See your gynaecologist for treatment.
iv) Genital warts
Genital warts are usually asymptomatic, but depending on their size and anatomic location, they can be painful, itchy, or cause cauliflower-like growths. They usually occur outside the vaginal and anus. They can appear in the vagina and around the cervix at times.
The diagnosis of genital warts is usually clinical, based on visual examination.
External warts (outside of the vagina) can be treated with a topical cream applied three times per week for six to 12 weeks. Internal vaginal warts or warts that do not respond to topical cream may necessitate laser vaporisation, which is a day surgery procedure performed under general anaesthesia.
Recent Blog Posts
- 20 August 2025
- 04 August 2025
- 07 July 2025
- 16 June 2025
- 16 June 2025
For a healthy start in life
For a healthy start in life
By Dr. Fong Kah Leng
Obstetrician and Gynaecologist
MBChB (Glasgow), MD (Singapore), FRCOG (UK)
Nutrition and weight management before and during pregnancy has a profound effect on the development of infants. This is a rather critical time for healthy fetal development as infants rely heavily on maternal stores and nutrient for optimal growth and health outcome later in life. Prenatal nutrition has a strong influence on birth weight and further development of the infant.
The "Barker Hypothesis", or thrifty phenotype, states that conditions during pregnancy will have long term effects on adult health. Associated risk of lifelong diseases includes cardiovascular disease, type-2 diabetes, obesity, and hypertension. Babies born lighter in weight appear to have an increased rate of mortality than babies born at a heavier weight. This does not mean that heavy babies are less of a concern. Death rate would rise as birth weight increases beyond normal birth weight range. Ideally, the rate of weight gain should be monitored during pregnancy to support the most ideal infant development. Eating a healthy diet is always a wise idea. Eat smart to cover any nutritional gaps in your diet.

Prenatal star supplements & superfoods
You are likely to be already on folic acid - one of the prenatal star supplements. Folic acid prevents malformations of the brain and spinal cord in babies and anaemia in pregnant women. A minimum of 600 mcg of folic acid per day during pregnancy can reduce the risks by as much as 70 per cent.
As the brain and spinal cord begin to form in the first trimester of pregnancy – before most women even know they are pregnant – women of childbearing age are to take a supplement containing folic acid daily, either as part of a multivitamin pill or as an individual nutrient, whether they are actively trying to get pregnant or not. Folic acid occurs naturally in green leafy vegetables, fruits, dried peas and beans.
Iron supplementation has been associated with a 50% reduction in the hazard for anaemia and a 19% reduction in the risk of low birth weight. Therefore, women who took iron supplements during pregnancy had a significantly lower risk of anaemia and low-birth-weight babies, according to a large meta-analysis.
During Pregnancy, iron needs increase per day. Thus, women should start taking prenatal vitamins that contain 30 mg of iron per day beginning with their first prenatal visit. Because this dose of iron can make some women nauseated or constipated, the prenatal vitamin should be taken with food (to minimize nausea) and to consume adequate fluids and high-fiber foods to cut down on constipation.
Docosahexaenoic acid (DHA), an omega-3 fatty acid, especially the kind found in fish, have been shown to be vital in normal brain and eye development and functioning in fetuses. It can also lower the risk of premature birth and increase the birth weight. There is also some evidence that supplementation might help prevent preeclampsia, postpartum depression, menopausal problems, postmenopausal osteoporosis and breast cancer. It also helps women avoid heart disease.
Almost all fish contain at least trace amounts of DHA, but salmon, herring, anchovies, and bluefin tuna are especially good sources of it. DHA is also found in some eggs, and fortified in some milks, cheeses, soymilks and snack foods such as cereal bars.
Choline is an important nutrient that helps brain cells develop properly. Animal studies suggest that adequate choline during pregnancy has long-lasting effects on a baby's ability to learn and remember – and may even provide some resistance to mental illness.
The recommendation for pregnant women is 450 mg of choline per day. You don't have to get the recommended amount of choline every day. Instead, aim for that amount as an average over the course of a few days or a week. Eggs, meat and fish are good sources of choline.

Prenatal exercises
The effect of exercise in pregnant women has been the subject of comprehensive research. Studies show that, in most cases, exercise is safe for both mother and fetus during pregnancy and they support recommendations to initiate or continue exercise in most pregnancies to derive the health benefits associated with such activities. It helps you cope and may even shorten your labour. More importantly, it helps you get back into shape after delivery.
If you have been exercising regularly before pregnancy, you should be able to continue all the way till delivery. Adapt your routines to your growing belly and listen to your body. If you have been a couch potato all this while, the recommendation is to start slow and easy, with 15-minute prenatal exercises three times a week, increasing gradually to 30-minute sessions four times a week, and finally to daily sessions. While exercise is generally safe for both mother and foetus during pregnancy, always remember to get the nod from your doctor before starting on an exercise regime while pregnant.
Women who have gestational diabetes mellitus must take particular precautions with exercise including monitoring blood glucose, regulating meal times, scheduling rest periods and carefully tracking fetal activity and uterine contractions.
No adverse effects on the fetus have been reported to occur during water exercise in pregnancy. The physiology of water exercise offers some compensation for the physiological changes of exercise on land that may beneficially affect pregnancy. If a woman is exercising in water (as in aquanatal classes) the water temperature should not exceed 32 degrees Celsius. Thirty-five degrees Celsius is the recommended maximum while using a hydrotherapy pool.
Women should stop exercising and seek medical advice should they feel unwell or experience any chest pain, vaginal bleeding, abdominal discomfort, reduced fetal movements etc.

Sounds
You have probably heard of the Mozart effect. It’s the idea that if babies listen to music composed by Mozart they will become more intelligent. A quick internet search reveals plenty of products to assist you in the task. There are CDs and books to help you to harness the power of Mozart’s music, but when it comes to scientific evidence that it can make you more clever, the picture is more mixed.
The Mozart Effect was a very popular study conducted by the University of California in 1993. The results of this study showed that college students who listened to the Austrian composer’s creations displayed an increase in IQ points in spatial reasoning. However, while music is recognised as a wonderful stimulation or relaxation tool, there is no solid evidence that you can increase your foetus’s future intelligence by playing music to it. While a daily dose of Mozart during pregnancy won’t make your baby a musical prodigy, he may recognise and be soothed by it when he hears it again as a newborn. It might also help you to relax, reduce stress and deepen your own feelings for your baby.
In the same way, your baby might also demonstrate that he recalls and is comforted by other noises heard while in the uterus. These could be the theme tune of your favourite TV programme (Hepper PG. 1988), or a story frequently read out loud to him (DeCasper AJ. et al. 1980). He may also prefer your voice, paying attention when you speak (DeCasper AJ. et al. 1980).
Don’t worry if you’re not comfortable with singing and chatting to your bump. The natural stimulation your baby receives from everyday conversations, and activities, is more than enough to prepare him for the outside world.
The above are positive steps to take to make pregnancy a wonderful experience – eat balanced meal, quit smoking, avoid alcohol, and give you and your baby a healthy start.
Recent Blog Posts
- 20 August 2025
- 04 August 2025
- 07 July 2025
- 16 June 2025
- 16 June 2025
Pregnancy diet: what to eat and what not to eat
Pregnancy diet: what to eat and what not to eat

A pregnant woman should always pay extra attention to what she eats, because the nutrients she gets also go to her baby. If mothers don't get enough of the right nutrients, it could affect how the baby grows and develops. The excess weight gain would also increase the risk of birth complications. Hence, consuming the proper nutrients would more likely ensure a healthy mom and baby!
Food you should eat during pregnancy
1. Fruit and vegetables
Fresh fruit and vegetables are the all-time foods that will never go wrong. They can be dried, frozen, fresh, or juiced. However, fresh and frozen fruits would have a higher level of vitamins and nutrients. For example, berries are packed with vitamin C, which is important for immune function. Dried fruits contain the same amount of nutrients as fresh fruits but without the water content. On the other hand, dark green vegetables also contain many nutrients that a pregnant woman needs. For example, spinach and kale are rich in vitamin k, vitamin c, calcium, fibre, and potassium.
2. Fibre
Pregnant women are more likely to experience constipation. You are highly encouraged to consume fibre to prevent it. The foods that are generally rich in fibre are wholegrains. Unlike refined grains, whole grains are packed with vitamin B and plant compounds. Quinoa and oats are also rich in protein. Other foods that are rich in fibre that you can consider eating during pregnancy are whole grain pasta, wholegrain bread, wild rice, beans, fruits, and vegetables.
3. Protein
The good sources of protein—lean meat, eggs, and fish—are particularly important for pregnant women. Lean meat like beef, pork, and chicken also provides high-quality protein. An egg contains almost every nutrient you need, including protein, fats, vitamins and minerals. Another important source that we can get from eggs is chlorine. It is essential for the brain development of the fetus.
What about if you are vegan? You can consider tofu, soy products, seeds, nuts, beans, quinoa, and legumes as great sources of protein.
4. Fats
Healthy fats, also called monounsaturated fats, are needed during pregnancy. A high-fat diet may cause future diabetes in babies. Hence, it is better that fats do not exceed 30% of your pregnancy diet. Foods high in monounsaturated fats include peanut oil, olive oil, sunflower oil, and avocado. Avocados are also high in vitamin C, vitamin E, vitamin K, copper, and fibre. The brain, tissues, and skin of the fetus would grow better if the mother ate healthy fats.
5. Iron
Pregnant mothers need more iron, which is the main part of haemoglobin. Extra iron is needed during pregnancy as a mother will increase almost 50% of the blood volume in her body, which requires more iron to make sure there is adequate oxygen supply for both mother and baby. Some foods that are rich in iron are salmon, cooked oysters, egg yolks, and poultry. Salmon is also rich in omega-3 fatty acids, which help to build the foetus’ brain and eyes.
Food you should avoid during pregnancy
1. High mercury fish
You may have heard that pregnant women need to avoid eating fish that contain high levels of mercury. This is due to the fact that it can pass through the placenta barrier and probably cause damage to the fetus. Since a growing baby's nervous system is still sensitive and developing, it is important to stay away from mercury to keep the baby's nervous system from getting hurt.
Marlin, swordfish, shark, yellowfin tuna, bigeye tuna, tilefish, orange roughy, and king mackerel are just some of the fish that are high in mercury.
2. Undercooked eggs
Raw or undercooked eggs are another thing mommy should avoid. Once you feel like having an egg, make sure it is cooked until the yolk and white are solid. Undercooked eggs can be a source of salmonella, which is a common cause of food poisoning. It is unlikely to harm the baby, but mommy may have a fight with diarrhoea and vomiting. On top of that, do avoid foods that include raw eggs. For example, mousse and mayonnaise.
3. Unpasteurized dairy product
In order to reduce the risk of food-borne illness, the next thing to avoid eating is unpasteurized dairy products, which includes goat milk and sheep milk. The same goes for soft cheese and unpasteurized milk, as they may contain bacteria called listeria. It probably shows no symptoms to the mother, but it can jeopardize the pregnancy by perhaps triggering miscarriage or premature birth.
4. Excessive vitamin A foods
We know that vitamin A is important for eye health, but if a pregnant woman gets too much vitamin A, her baby could be born with birth defects. What an expectant mom can do is to avoid eating liver or liver products. If you are deficient in vitamin A, it is best to seek the advice of a doctor and get their advice on supplementation. The safest way to do this is to consult a professional before taking any multivitamins.
Going through the pregnancy journey is not an easy job, but it is worth it when your little one gets the best and always stays healthy. After delivering your new-born, it’s time to take note of your post-natal diet. Although there is still some food to avoid, there is also amazing food waiting for you!
Ever wondered how these 7 popular confinement food ingredients will help you recover after giving birth?

Recent Blog Posts
- 20 August 2025
- 04 August 2025
- 07 July 2025
- 16 June 2025
- 16 June 2025
Pagination
- Page 1
- Next page

